Avoiding complications during osteoporosis treatment
Percutaneous vertebroplasty involves injecting a so-called bone cement into the vertebrae of patients suffering from osteoporosis. The treatment is minimally invasive: the surgeon gradually injects a few milliliters of the bone cement whilst continuously MRI images of the patient’s brain, to determine the best fit and, at the same time, most physically useful, meaningful parameters”, Koch explains. This process is done automatically, whereby the most relevant parameters are those that describe the physical properties of the materials. For instance, diffusion coefficients for the capillary walls can be found in the scientific literature or from the geometry of the capillaries. “A total of about ten parameters used in our model have an influence on the calculations”, says Koch.
“The concentration profile with which the contrast medium moves through the capillaries is ultimately unknown, which means that you have to play through a reasonable range of values”. Finally, the researcher has to merge the flow model with the MRI images. Only then can useful conclusions be drawn about the development of the lesions. To this end, Koch also models the MRI imaging in a subordinated simulation. In this way, the researchers hope to gain a better understanding of the flow processes of an MS sufferer’s brain than can be achieved with existing models. Special research for porous media The technical know-how about porous media available in Stuttgart is not just a reflection of Koch’s research. In autumn 2017, the University received approval for a German Research Foundation (DFG) collaborative research center (CRC) focused on “boundary surface-driven multi-field processes in porous media”. Over 20 scientists from several of the University’s institutes participate in checking the results with x-ray images. “It’s a standard treatment”, says Röhrle, “but, unfortunately, complications, such as bone cement leaking out of the vertebra, do occur from time-to-time. Moreover, the surgeon never knows how the bone cement will alter the mechanical behavior of the human musculoskeletal system”. Ultimately, the patient’s vertebrae, ligaments, tendons and muscles will have adapted to the altered structure of the backbone. “Then there’s the fact that, in the final analysis, the injected bone cement spreads differently in every patient”.

Photo: University Stuttgart / Max Kovalenko
„It’s a standard treatment, but, unfortunately, complications, such as bone cement leaking out of the vertebra, do occur from time-to-time. Moreover, the surgeon never knows how the bone cement will alter the mechanical behavior of the human musculoskeletal system.“
Oliver Röhrle, Professor for Continuum Biomechanics and Mechanobiology at the University of Stuttgart.
From a fluid mechanics perspective, percutaneous vertebroplasty is a typical example for the processes in porous media. The injected bone cement sets within the vertebra, so that when it first enters the bone it causes a volume change and then, after setting results in a phase change from fluid to solid. “We’re trying to use simulations to describe these processes”, says Röhrle. And, at the same time, to take account of the properties of at least three materials – bone, bone marrow and bone cement. To validate the Stuttgart model, the scientists will be collaborating with the AO Research Institute Davos. “They have experimental laboratory set-ups there as well as the clinical problems that we require for our model development”, Röhrle explains. Only once the results of this first phase are available will the project participants be able to approach the question in which they are really interested: what exactly happens when a vertebra breaks or cracks?
— Michael Vogel (Forschung Leben, Ausgabe 11/2018)
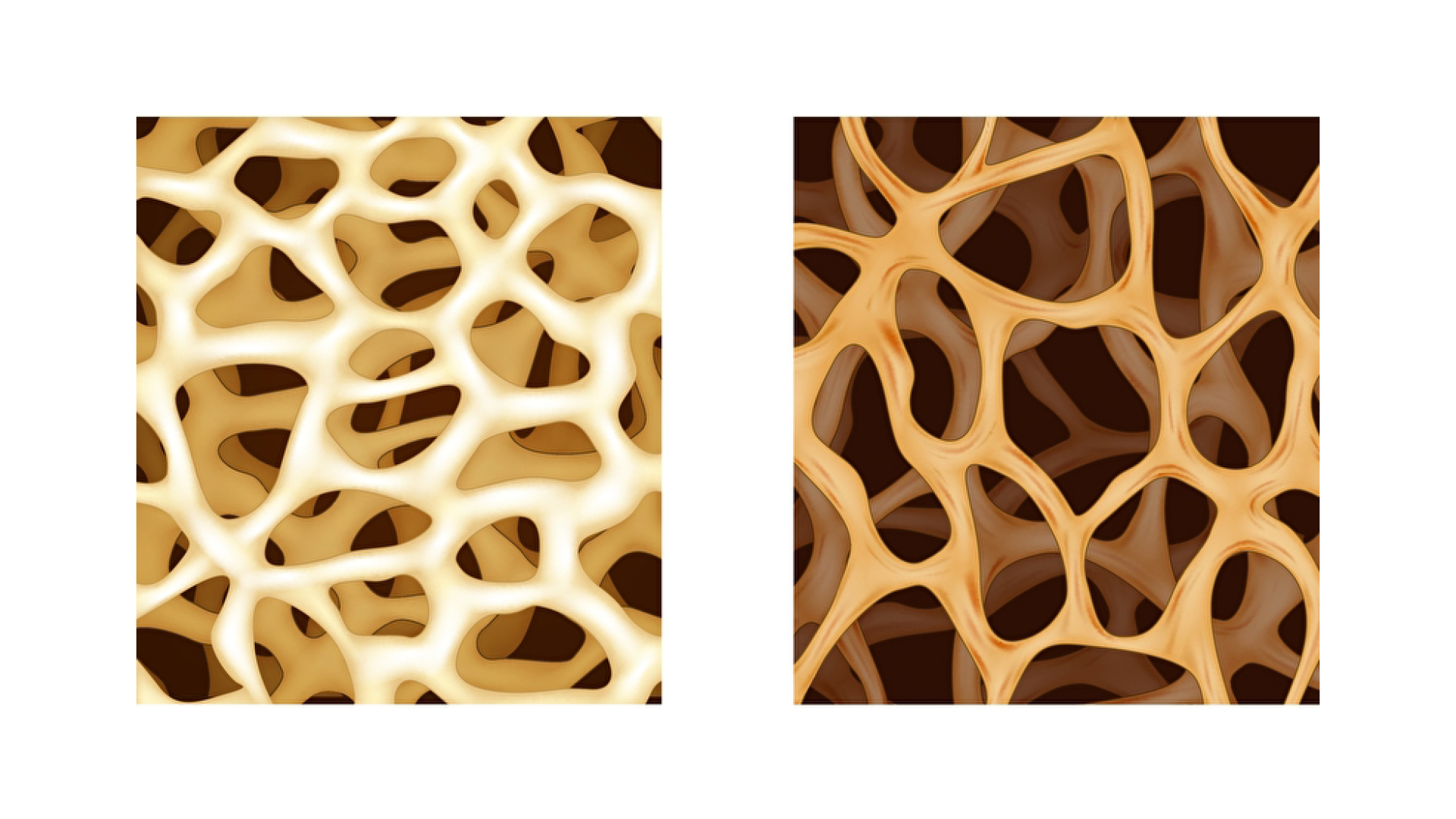
As we age, our bones lose their bone mass. That means that the density drops, their cavities become larger and the stability of the bones decreases. This disease is called osteoporosis. Osteoporosis therefore often results in bone fractures.
Credits: PantherMedia / Teguh Mujiono
Credits: PantherMedia / Artemida-psy und rob3000
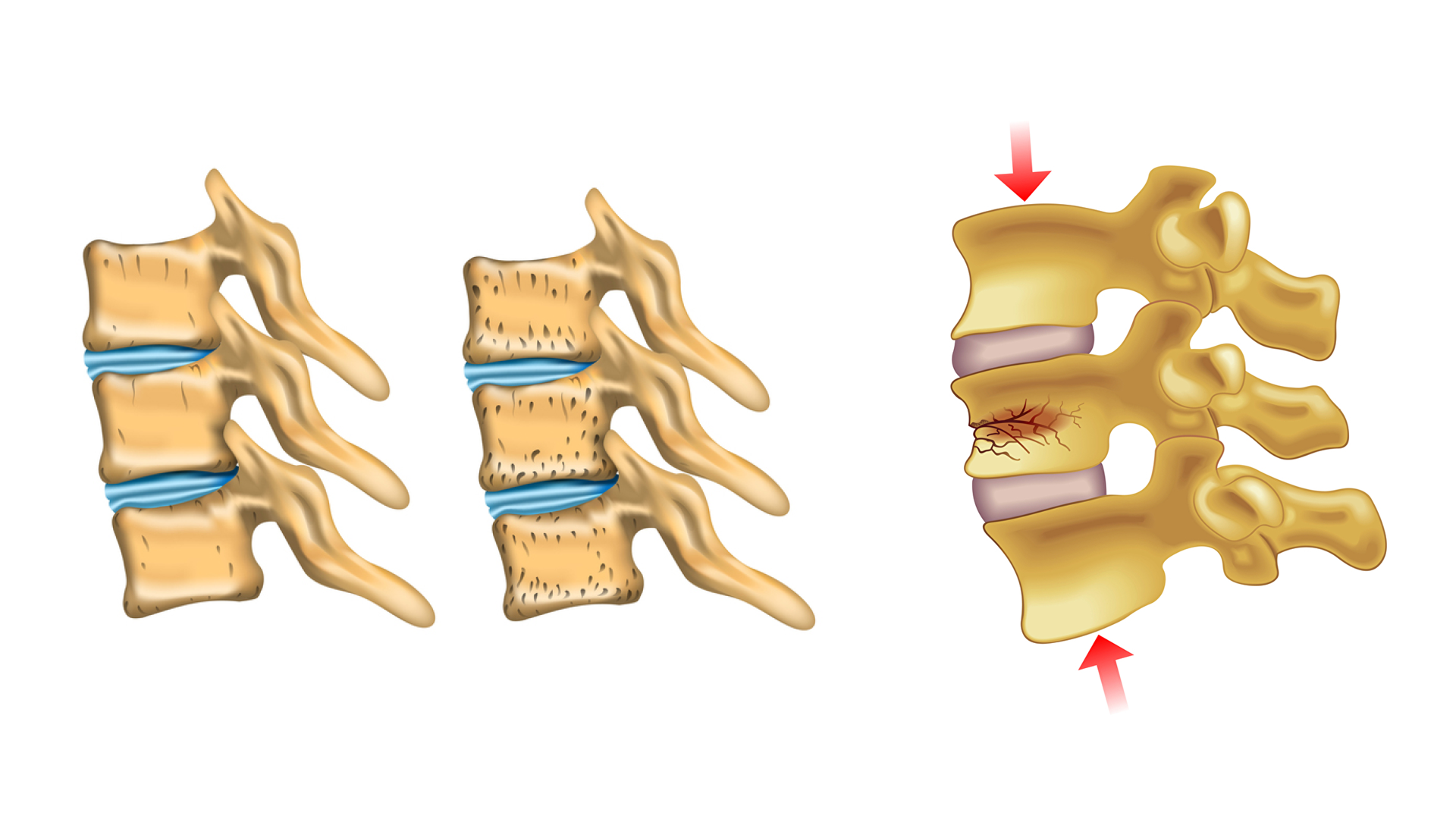
Stabilization of fractured vertabrae
One of the procedures for stabilisation of (fractured) vertabrae is the so-called “percutaneous vertebroplasty”. This treatment method allows physicians to “refill” and stabilize the bone by injecting the so-called “bone cement” into the vertebrae of patients suffering from osteoporosis. Step by step, few milliliters of bone cement are injected while repeatedly checking the spread of the bone cement by means of X-rays. The “liquid” bone cement hardens within approximately 20 minutes and stabilizes the bone.
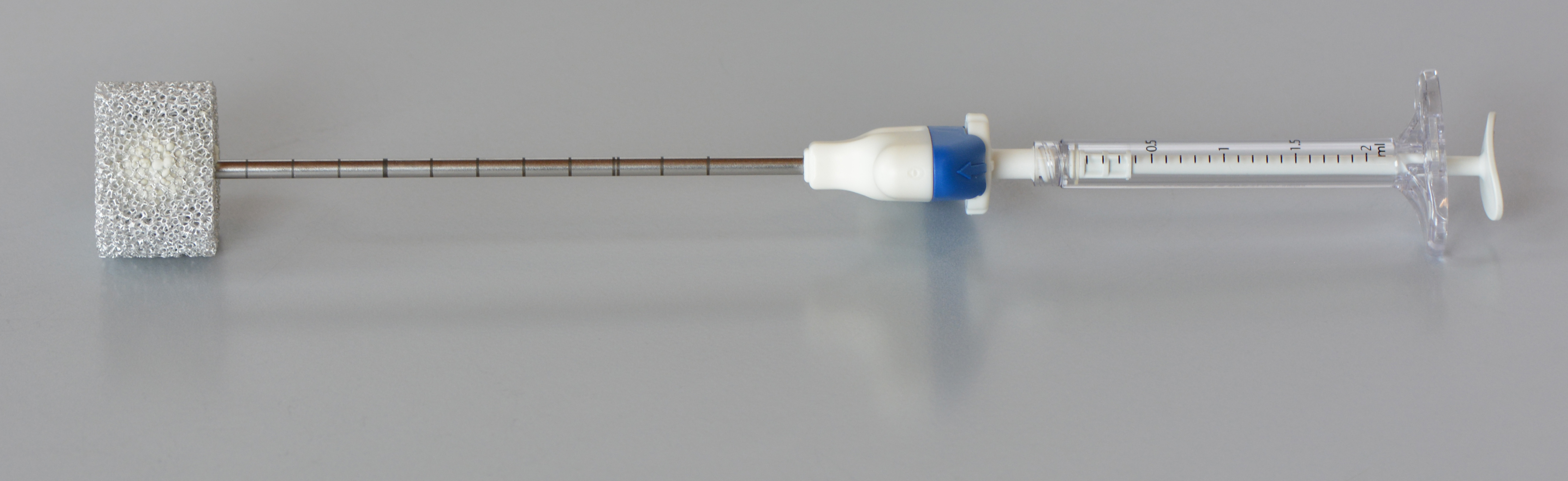
Credits: AO Foundation Davos / Dominic Gehweiler
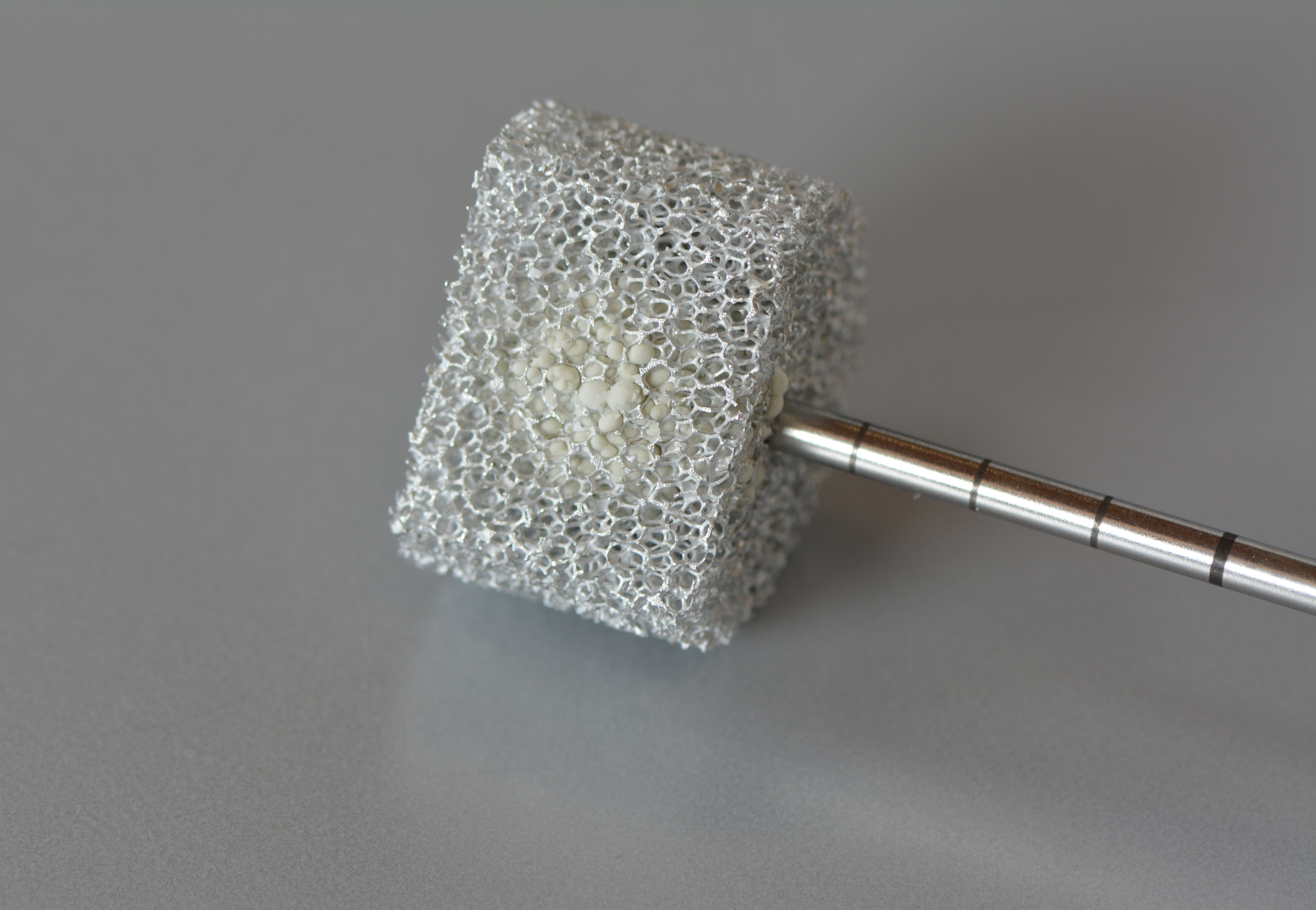
Credits: AO Foundation Davos / Dominic Gehweiler
Credits: AO Foundation Davos / Dominic Gehweiler
Credits: AO Foundation Davos / Dominic Gehweiler
International cooperation
The University of Stuttgart* in collaboration with the AO Research Institute Davos* (Switzerland) perform joint research in this field. Scientists at the University of Stuttgart use the experimental data from Davos to generate simulations. This knowledge can help physicians to better understand vertebroplasty and improve this treatment method. Furthermore, these simulations are also important to detect and avoid possible complications (e.g. bone cement leakage, damage to the nerves in the spine, etc.).
*Oliver Röhrle (University of Stuttgart) / Boyko Gueorguiev-Rüegg (AO Foundaitio, Davos)
Credits: AO Foundation Davos / Dominic Gehweiler
Credits: University of Stuttgart / Christian Bleiler
In-depth text of the simulation of a bone cement infection and the spread of the mass.
Bone cement spreading during vertebroplasty
The human skeleton goes through a lifelong process called bone tissue remodelling, in which mature bone tissue is removed and replaced by newly formed tissue. If this process is no longer in equilibrium and bone tissue does not grow in sufficient quantities, it will lead to bone shrinkage and a decrease of bone density. This disease, which often occurs in old age, is called osteoporosis and can lead to massive restrictions in the stability of the entire skeleton and can be associated with a greatly increased risk of bone fractures. In the area of the spine, the weakening of the bone structure can lead to sintered fractures in the vertebral bodies and to serious complaints from those affected. Vertebroplasty is a therapeutic treatment to stabilize osteoporotic vertebral bodies and represents a minimally invasive operation, in which so-called bone cement is injected percutaneously into the vertebral body and stabilizes it again after the previously liquid bone cement has hardened. During the treatment, particular care must be taken to ensure that no injection material emerges from the vertebral body. Possible serious consequences caused by cement leakage are an embolism or a compressing of the spinal cord.
Eine Therapiemaßnahme zur Stabilisierung von osteoporotischen Wirbelkörpern ist die Vertebroplastie. Dies ist eine minimalinvasive Operation, bei welcher sogenannter Knochenzement in den Wirbelkörper perkutan injiziert wird und diesen nach dem Aushärten des zuvor flüssigen Knochenzements wieder festigt. Bei der Operation muss insbesondere darauf geachtet werden, dass kein Injektionsmaterial aus dem Wirbelkörper austritt. Mögliche schwerwiegende Folgen einer solchen Zementleckage sind etwa das Verursachen einer Embolie oder die Kompression des Rückenmarks.
The numerical simulation of vertebroplasty can help to avoid complications during the procedure and to make predictions about the spreading of the bone cement within the vertebral body. The main goal here is to optimize the process of treatment by testing factors such as the position of the injection needle, the choice of bone cement and the necessary injection pressure in preoperative simulations. On the one hand, this gives surgeons the opportunity to assess risks in advance and, on the other hand, to achieve the best possible therapy result. Another goal in simulating vertebroplasty is to gain a deeper understanding of the forces and pressures that arise within the vertebral body during bone cement injection. This enables predictions to be made as to whether the trabecular bone structure is deformed or destroyed by the resulting stresses caused by the injection.
The employed continuum mechanical model is based on the Theory of Porous Media (TPM) and relies on the formulation of constitutive relations for the solid skeleton of the bone, the injected bone cement and the bone marrow, which fills the bone at the beginning. This enables the direct consideration of important parameters such as the bone cement viscosity and the anisotropic permeability of the bone structure in the vertebra. The resulting system of equations is solved in a fully coupled manner and allows the simultaneous investigation of the injection process and the spreading of the bone cement with the associated displacement of the bone marrow and the resulting stresses and deformations within the bone structure.
Credits: University of Stuttgart / Christian Bleiler
Pretty Porous
04
04
Biology
If we take a close look at ourselves, we recognize that we are essentially a porous medium too – Whether our skin, brain, human cells, arteries and veins, or even bones.
Credits: University of Stuttgart / VISUS / Stefan Scheller
Credits: Natalie Weinman, Sven Tillack, Steffen Knöll
Using the example of the porous bone structure, we show what is osteoporosis (bone mass loss) and how its symptoms can be eased.